Healthcare organizations face mounting pressure to improve patient safety while optimizing operational efficiency. According to the Agency for Healthcare Research and Quality, medication errors harm approximately 1.5 million patients annually in the United States alone, with associated costs exceeding $3.5 billion. QR codes offer a practical solution that transforms workflows across patient identification, medication administration, specimen tracking, and asset management without requiring the significant infrastructure investment of alternatives like RFID.
Modern smartphones scan QR codes natively while EHRs and ancillary systems increasingly support barcode and QR workflows through standards like HL7 FHIR. Compared to linear barcodes, QR codes encode more data, scan reliably even when partially obstructed, and work with devices already in clinicians' hands. The result is faster verification, fewer errors, and better documentation without adding friction to clinical workflows already burdened by technology demands.
This guide covers the core use cases transforming healthcare operations, security and compliance considerations essential for HIPAA compliance, implementation strategies that minimize disruption, and measurement frameworks that demonstrate ROI to justify investment.

Transform Healthcare Workflows with QR Analytics
VISU powers real-time scan tracking, secure routing, compliance logs, and multi-location analytics for healthcare organizations.
Why QR Codes in Healthcare, Why Now?
Several converging factors make this the optimal moment for healthcare QR adoption. Native camera scanning on iOS and Android eliminates the need for dedicated hardware procurement. Patient expectations for self-service and mobile experiences continue rising after pandemic-accelerated digital adoption. Quality and safety initiatives from organizations like The Joint Commission focus increasingly on medication accuracy and identity verification. Interoperability standards like HL7 FHIR and SMART on FHIR provide frameworks for secure data exchange that were unavailable a decade ago.
The operational impact spans multiple areas simultaneously. Medication errors decrease through mandatory bedside verification that cannot be bypassed. Patient queues shrink with mobile check-in that starts in the parking lot. Asset utilization improves through real-time tracking that reveals where equipment actually sits. Documentation becomes more robust with automated timestamps and audit trails that satisfy regulatory requirements.
Organizations implementing comprehensive QR tracking report 40 to 60 percent reductions in medication administration errors, 25 to 35 percent improvements in equipment utilization, and 15 to 20 percent decreases in patient wait times. These metrics directly impact both safety outcomes and financial performance through reduced adverse events, better asset ROI, and improved patient satisfaction scores that increasingly affect reimbursement.
Core Use Cases That Deliver Measurable Value
QR codes deliver quantifiable value across six critical healthcare workflows. Each use case generates distinct performance metrics that inform targeted improvements and justify continued investment.
Patient Identification and Wristband Verification
Wristband QR codes encode MRN and encounter information while linking to allergies, alerts, and consent status stored in the EHR. Staff scan at triage, imaging, surgical centers, and medication administration to prevent wrong-patient events that remain a persistent source of serious harm. When integrated with the EHR, scanning can launch contextual applications directly from the wristband, eliminating navigation through multiple screens.
Key performance indicators include wrong-patient events per thousand encounters, average ID verification time, and scan success rate across lighting conditions and wristband wear states. A 450-bed hospital system reduced patient ID errors by 73 percent within six months by using scan analytics to identify high-risk scenarios including shift changes, float staff assignments, and emergency admissions. Targeted interventions for these specific scenarios addressed the majority of residual risk.

Medication Administration and BCMA Compliance
QR codes on medication labels support five-rights checking at the bedside: right patient, right drug, right dose, right route, right time. Integration with the EHR enables automatic documentation in the Medication Administration Record, eliminating manual charting that delays nurses and introduces transcription errors. Alerts flag lot and expiration discrepancies before administration occurs.
Performance metrics include BCMA adherence rate, near-miss event rates, and scanning reliability across conditions including low light and medication packaging variability. Analytics consistently reveal that 80 percent of BCMA workarounds occur during specific high-pressure scenarios: code situations, nurses managing multiple simultaneous patients, and EHR system downtime. Targeted training and process redesign for these scenarios eliminates the majority of risky behaviors while avoiding blanket policies that create frustration.
Laboratory Specimens and Chain of Custody
QR labels link specimens to orders, patients, and collection timestamps from the moment of draw. Scans during transport and processing preserve chain of custody with automated documentation that satisfies regulatory requirements. Any break in the expected chain triggers immediate alerts to laboratory supervisors.

Key indicators include specimen relabeling incidents, turnaround time by test type, and collection-to-result accuracy rates. A regional lab network reduced stat test turnaround time by 28 percent by using QR analytics to identify transport delays between collection sites and central processing. Courier route optimization based on actual scan data rather than assumptions about traffic patterns delivered immediate improvement.
Medical Equipment and Asset Tracking
QR tags on equipment display manuals, maintenance schedules, and quick-start guides through a single scan. Integration with computerized maintenance management systems plus location data from scan patterns reduces losses and increases utilization. Staff spend less time searching for equipment and more time providing care.
Performance metrics include time to locate critical equipment, preventive maintenance compliance rates, and equipment loss rates. A 300-bed hospital avoided $1.2 million in planned IV pump purchases by using QR tracking analytics to discover that 30 percent of existing pumps were sitting unused in storage areas, hallways, and non-clinical spaces. Redistribution based on actual utilization data solved the perceived shortage without capital expenditure.

Patient Onboarding and Registration
QR codes at registration kiosks and on appointment reminders enable patients to complete check-in from their own devices. Mobile check-in reduces queues while automatically updating demographic data that patients correct themselves rather than requiring staff verification. Portal activation increases through frictionless enrollment that happens during the natural flow of a visit.
Key indicators include average registration time, demographic data accuracy rates, and patient portal activation rates. Outpatient clinics using QR-based pre-registration reduce front-desk staffing needs by 30 to 40 percent while improving patient satisfaction scores related to wait times and perceived efficiency.
Discharge Instructions and Post-Visit Engagement
QR codes on discharge paperwork direct patients to personalized video instructions, medication guides, and follow-up scheduling. Patients access information when they need it rather than trying to remember verbal instructions from a stressful hospital discharge. Analytics reveal which instructions patients actually access, enabling continuous improvement.

A large medical center reduced missed follow-up appointments by 12 percent by analyzing QR wayfinding data to identify that patients were arriving for appointments on time but getting lost before reaching their destination. Parking garage signage was inadequate, and the subsequent navigation confusion caused patients to give up and leave.
Safety, Compliance, and Security Requirements
QR code implementations in healthcare require careful attention to privacy, security, and regulatory compliance. Proper design protects patient information while enabling the operational benefits that justify investment.
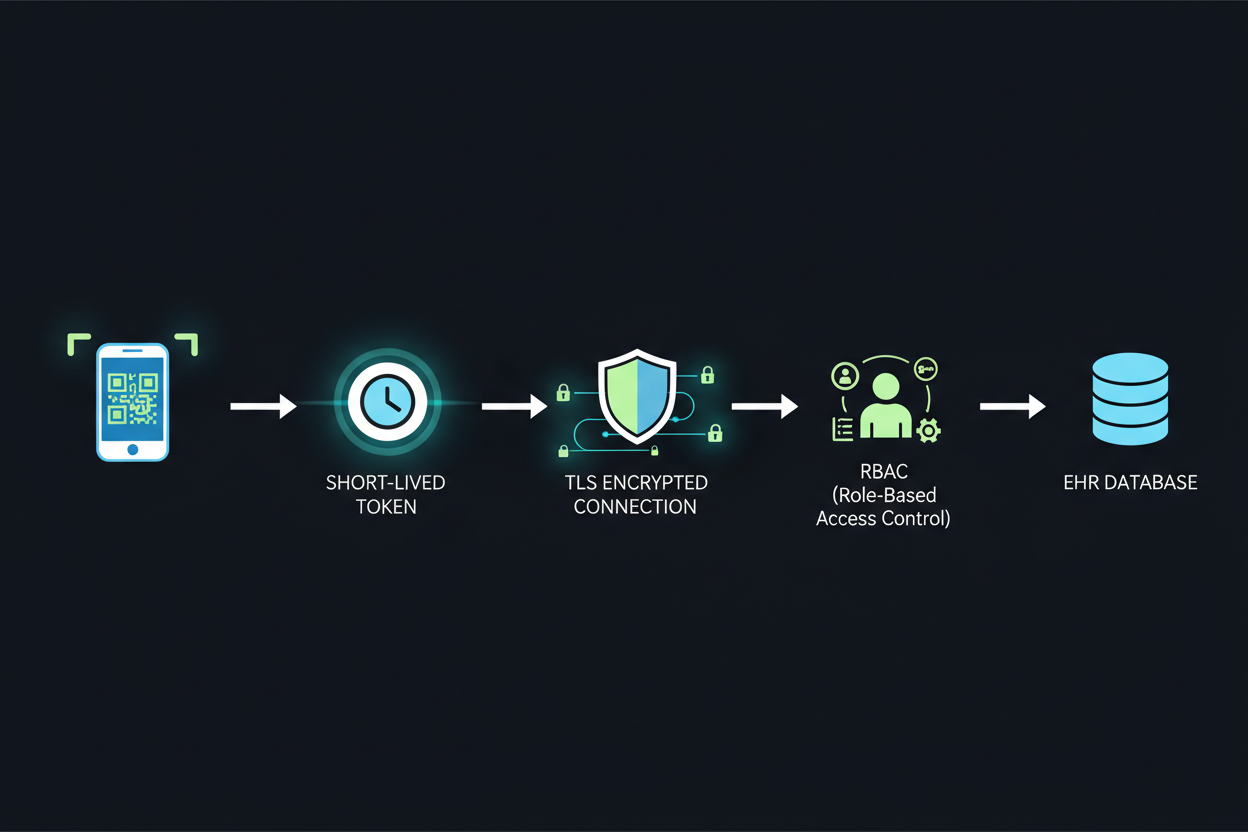
PHI Minimization and Token-Based Architecture
Never encode protected health information directly in QR payloads. Instead, use short-lived tokens that require authentication to resolve to actual patient data. Tokens expire after use or after a defined time window, limiting exposure if codes are photographed or shared inappropriately. This architecture satisfies HIPAA minimum necessary requirements while maintaining workflow efficiency.
Authenticity Verification and Anti-Tampering
Signed QR codes for medications and documents prevent substitution attacks that could direct staff to incorrect information. Digital signatures verify that codes originate from authorized sources within the healthcare system. Any modification to the code payload invalidates the signature, triggering alerts.
Accessibility and Inclusive Design
High-contrast codes accommodate patients and staff with visual impairments. Alternative pathways must exist for patients without smartphones or with limited technical comfort. Voice-assisted scanning and large-format codes in key locations ensure QR benefits extend to all patient populations.
Consent and Privacy Transparency
Clear notices explain how QR interactions may personalize care and what data is collected. Patients should understand before scanning whether their interaction is logged and how that information will be used. Consent mechanisms should be as frictionless as the scanning itself.
Implementation Blueprint: Pilot to Enterprise Scale
Successful QR implementations follow a structured approach that proves value quickly while building toward enterprise-wide adoption. Rushing to scale before validating workflows creates adoption resistance that is difficult to overcome.

Phase 1: Strategy and Objective Definition
Start by defining clear, measurable KPIs such as 30 percent improvement in BCMA adherence or 50 percent reduction in equipment search time. Map existing workflows in detail and identify integration points with current EHR, WMS, and CMMS systems. Choose a tokenized payload approach that protects PHI while enabling the analytics needed to demonstrate value.
Phase 2: Pilot Unit Selection and Configuration
Select a pilot unit with engaged leadership and manageable complexity. Medical-surgical units often work well as initial pilots due to predictable workflows and significant medication administration volume. Integrate via FHIR and HL7 standards for maximum interoperability with existing systems. Train super users who will support colleagues during initial adoption.
Phase 3: Measurement and Iteration
Measure results over 6 to 8 weeks before considering expansion. Collect both quantitative metrics and qualitative feedback from frontline staff. Iterate on label design, scanner configuration, and workflow integration based on real usage data. Problems identified during pilot are much cheaper to solve than problems discovered after enterprise rollout.
Phase 4: Scaled Rollout
Expand in waves, using pilot champions as trainers and advocates in new departments. Maintain measurement discipline as new units onboard. Expect some variation in adoption patterns across different clinical cultures and adjust support accordingly.
Organizations that invest in comprehensive training and change management see three times higher adoption rates than those that focus only on technology deployment. The technology is the easy part; changing clinical behavior requires sustained attention.
ROI Framework and Financial Justification
QR tracking investments typically achieve positive ROI within 12 to 18 months through multiple value streams that compound over time.

Primary Value Drivers
Errors prevented represent the highest-value category, with each prevented adverse drug event saving $2,000 to $8,500 in direct costs plus avoiding potential liability. Labor time saved aggregates across all scanning touchpoints, with typical BCMA implementations saving 15 to 20 minutes per nurse per shift. Asset utilization improvements delay capital purchases and reduce rental costs. Patient throughput increases generate additional revenue from the same fixed infrastructure. Satisfaction score improvements increasingly affect reimbursement under value-based payment models.
Measurement Cadence and Governance
Establish weekly KPI reviews during pilot and early rollout phases. Monthly adherence assessments identify departments or individuals needing additional support. Quarterly ROI calculations build the business case for expansion and sustain executive sponsorship. This measurement rhythm ensures problems are caught early while building the data needed to justify enterprise investment.
Sample ROI Calculation
A representative 300-bed hospital implementing BCMA-focused QR tracking shows investment of $250,000 covering software licensing, implementation services, training, and supplemental scanning devices. Annual benefits include medication errors prevented at $675,000, nursing time saved at $360,000, pharmacy waste reduction at $85,000, and compliance risk mitigation valued at $120,000. Total annual benefit reaches $1.24 million, yielding first-year net ROI of 396 percent with payback period under three months.
Common Implementation Pitfalls to Avoid
Organizations implementing healthcare QR systems encounter predictable challenges. Anticipating these pitfalls enables proactive mitigation rather than reactive firefighting.
Encoding PHI Directly in QR Codes
This creates compliance risk and security vulnerabilities that can result in HIPAA penalties and reputational damage. Use tokenized references that expire and require authentication to resolve to patient data.
Choosing Low-Durability Label Materials
Standard labels fail quickly in clinical environments with frequent cleaning, handling, and chemical exposure. Scanning failures frustrate staff and create workarounds that defeat the purpose of the system. Invest in medical-grade materials rated for expected environmental conditions.
Implementing Without Workflow Mapping
Forcing staff to work around the system rather than with it creates resistance and poor adoption. Map processes in detail before implementation and redesign workflows as needed to make scanning the path of least resistance.
Insufficient Training and Change Management
Brief demonstrations are not training. Staff need hands-on practice with real clinical scenarios, including exception handling for situations where scanning fails or produces unexpected results. Ongoing support during the first weeks of use prevents early frustrations from becoming permanent resistance.
Inadequate Device Ratios
Creating bottlenecks when staff must share scanners or wait for equipment undermines the efficiency gains that justify investment. Budget for sufficient devices at appropriate ratios for each workflow type, recognizing that different clinical areas have different scanning densities.
Future Outlook: Emerging Capabilities
Healthcare QR applications continue evolving with emerging technologies and standards that will expand capabilities over the next three to five years.
SMART on FHIR Deep Linking
QR codes will launch specific EHR contexts directly, eliminating multiple navigation steps. Scanning a patient wristband will open directly to the relevant medication list or order entry screen rather than requiring manual navigation.
Verifiable Credentials for Patient-Held Records
Patients will present vaccination records, insurance information, and advance directive status via QR codes stored on their phones, with cryptographic verification of authenticity. This shifts control to patients while reducing administrative burden on healthcare organizations.
NFC and QR Hybrid Approaches
Tap-or-scan flexibility will accommodate different device capabilities and user preferences. Some workflows will favor the speed of NFC tap while others will benefit from the distance and visual confirmation of QR scanning.
AI-Powered Triage via QR Entry Points
QR codes will direct patients to symptom assessment tools that use AI to route to appropriate resources based on acuity and care needs. This extends clinical decision support to the front door of healthcare encounters.
Organizations investing in QR infrastructure today position themselves to adopt these capabilities as they mature, building on existing workflows and staff familiarity rather than starting over with each new technology wave.
Bring QR Analytics to Your Healthcare Workflow
VISU powers real-time scan tracking, secure routing, compliance logs, and multi-location analytics for healthcare organizations of all sizes.